
Herniated Discs and Sciatica Explained
What if understanding a common source of pain could empower you to take control of your health? Herniated discs and their relation to sciatica are often misunderstood, yet grasping their impact can transform your recovery journey.
What You Will Learn
- A herniated disc occurs when the inner gel protrudes through the outer layer, potentially compressing nerves and causing pain.
- Common symptoms of a herniated disc include sharp pain, tingling, or weakness in the legs, often associated with sciatica.
- Effective treatment options range from physical therapy to surgical interventions, depending on the severity of the condition.
- Maintaining healthy intervertebral discs is essential for spine health, supporting mobility, flexibility, and alignment.
- Rehabilitation plays a key role in recovery from sciatica, enhancing function and reducing the risk of future episodes.
- Incorporating targeted stretching and strengthening exercises can alleviate pain and build resilience around the spine.
Sciatica Recovery: Milestones and Rehabilitation
Understanding the typical recovery timeline and the crucial role of rehabilitation can help manage expectations for sciatica sufferers.
Understanding Herniated Discs and Their Impact on Sciatica
Herniated discs are a common source of discomfort for many individuals suffering from sciatica. Understanding what a herniated disc is and how it affects your body can empower you to make informed decisions about your health. Have you ever felt a sharp pain radiating down your leg? This discomfort often stems from issues related to the discs in your spine, which serve as crucial shock absorbers.
In essence, a herniated disc occurs when the soft inner gel of the disc protrudes through the outer layer, potentially pressing on nearby nerves. This can lead to a variety of symptoms, including pain, numbness, or weakness in the legs. At Sciatica Solutions, we strive to provide resources that help demystify these complex conditions, ensuring you understand the root of your pain.
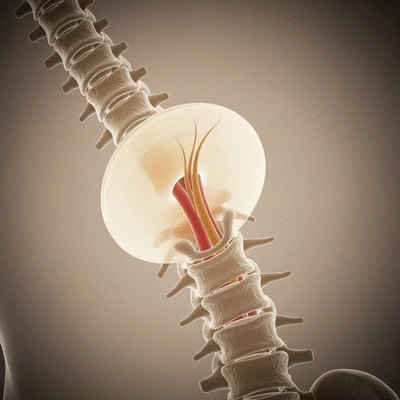
What is a Herniated Disc?
A herniated disc, sometimes referred to as a slipped or ruptured disc, is a condition where the intervertebral disc's outer layer tears, allowing the inner material to bulge out. This bulging can irritate nearby nerves, resulting in pain and other symptoms. It’s important to recognize that herniated discs can occur in any part of the spine, but they are most common in the lumbar region.
- Causes: Herniated discs can result from wear and tear due to aging, injury, or repetitive stress on the spine.
- Symptoms: Symptoms often include sharp pain, tingling, or weakness in the affected leg. For a detailed understanding of the clinical presentation, you can refer to authoritative medical sources, such as this article on Lumbar Disc Herniation from NCBI Bookshelf.
- Treatment Options: Options range from conservative management like physical therapy to surgical interventions in more severe cases.
By understanding the nature of herniated discs, you can better approach your treatment options and recovery plans. If you're experiencing pain, it's essential to consult with a healthcare professional to determine the best course of action.
The Anatomy of the Lumbar Spine: Key Structures Involved in Sciatica
The lumbar spine is a complex structure made up of vertebrae, intervertebral discs, nerves, and surrounding muscles and ligaments. Understanding this anatomy is crucial when exploring how herniated discs can lead to sciatica. The lumbar region consists of five vertebrae (L1-L5), with intervertebral discs situated between them, acting as cushions.
When a herniated disc occurs in the lumbar spine, the nerves that exit through the openings between these vertebrae can become compressed. This compression can cause pain that radiates along the sciatic nerve, a long nerve that runs down the back of your legs. Recognizing the structures involved helps clarify the link between herniated discs and sciatica, as further elaborated in this review on lumbar disc herniation and radiculopathy.
Role of Intervertebral Discs in Spine Health
Intervertebral discs play a vital role in maintaining spine health. They provide flexibility and support to the spine, allowing for movements such as bending and twisting. When these discs become damaged, as in the case of a herniation, it not only affects mobility but can also lead to significant pain and discomfort.
- Shock Absorption: They absorb shock during daily activities like walking, running, and lifting.
- Maintaining Spinal Alignment: Discs help keep the vertebrae aligned, which is essential for overall posture and balance.
- Facilitating Movement: Healthy discs allow for a full range of motion, which is crucial for an active lifestyle.
Ultimately, maintaining the health of your intervertebral discs is crucial for preventing conditions like sciatica. By focusing on core strength and proper body mechanics, you can help protect these important structures and support your spinal health.
How Herniated Discs Cause Sciatica: A Closer Look at Pathophysiology
Now that we’ve established an understanding of herniated discs and their anatomy, let’s delve deeper into how these conditions specifically lead to sciatica. The connection between the two is critical for understanding your symptoms and treatment options.
In the next sections, we'll explore the mechanisms behind nerve root compression, common locations for herniated discs, and the concept of radiculopathy as it relates to herniated discs. Understanding these factors will equip you with the knowledge to discuss your concerns with healthcare providers and make informed decisions about your treatment journey.
Did You Know?
According to a study published in the Journal of Pain Research, approximately 90% of individuals with sciatica related to herniated discs experience significant improvement in their symptoms within six weeks, especially with appropriate rehabilitation strategies. This highlights the importance of early intervention and a tailored treatment plan!
Long-Term Prognosis and Rehabilitation for Sciatica Sufferers
Recovering from sciatica related to herniated discs can feel like a daunting journey. However, understanding the long-term prognosis is crucial. Many patients experience significant improvement in their symptoms over time, especially with appropriate treatment and rehabilitation. It's important to remember that while some individuals may see quick relief, others might need a more gradual approach to recovery.
When managing expectations, it's vital to recognize that recovery is not always linear. You might have good days and bad days, but consistency in following your treatment plan can yield positive results!
Managing Expectations: Recovery Post-Treatment
- Initial recovery may take several weeks to months.
- Many patients report substantial pain relief within the first few weeks after starting treatment.
- Full recovery can take anywhere from three months to a year, depending on individual circumstances.
- Regular check-ins with your healthcare provider can help monitor progress and adjust treatment plans.
After treatment, it's crucial to maintain realistic expectations about your recovery timeline. Understanding these factors can empower you to stay engaged and proactive during your healing journey.

Importance of Rehabilitation and Functional Recovery
Rehabilitation plays a pivotal role in ensuring a successful recovery from sciatica. Engaging in a structured rehabilitation program helps restore function, improve mobility, and reduce the risk of future episodes. According to my experience at Sciatica Solutions, patients who actively participate in rehabilitation tend to achieve better outcomes.
Rehabilitation can involve various components, such as:
- Education about body mechanics and posture.
- Progressive exercises tailored to individual needs.
- Manual therapy to relieve pain and improve function.
- Guidance on activities of daily living to avoid further strain.
By focusing on rehabilitation, we can help our patients regain not just their physical health but also their confidence in movement!
Stretching and Strengthening Exercises for Sciatica Relief
One of the most effective ways to manage sciatica symptoms is through targeted exercises. Stretching and strengthening can alleviate pain and prevent future injuries. At Sciatica Solutions, I often recommend the following exercises:
- Piriformis Stretch: Targets the muscle that can irritate the sciatic nerve.
- Knee-to-Chest Stretch: Helps relieve tension in the lower back.
- Bridges: Strengthens the glutes and lower back, supporting spinal alignment.
- Cat-Cow Stretch: Promotes flexibility and mobility in the spine.
Incorporating these exercises into your routine can enhance recovery and build strength around your spine. Always consult with a healthcare professional before starting any new exercise program to ensure it aligns with your specific needs. For more insights on the effectiveness of non-surgical treatments, including rehabilitation and exercises, you can read this review on conservative management of lumbar disc herniation.
Frequently Asked Questions About Herniated Discs and Sciatica
What exactly is a herniated disc?
A herniated disc occurs when the soft, gel-like inner material of an intervertebral disc pushes through a tear in its tougher outer layer. This can compress nearby nerves, leading to symptoms like pain, numbness, or weakness.
How does a herniated disc cause sciatica?
When a herniated disc occurs in the lumbar (lower back) region of the spine, it can press on the nerve roots that form the sciatic nerve. This compression irritates the nerve, causing pain that radiates along its path, which is known as sciatica.
What are the common symptoms of a herniated disc and sciatica?
Common symptoms include sharp, radiating pain down the leg, often accompanied by tingling, numbness, or muscle weakness in the affected limb. The pain can range from a dull ache to a sharp, burning sensation.
What are the typical recovery timelines for sciatica caused by a herniated disc?
Initial improvement can often be seen within a few weeks of starting treatment. Full recovery can vary significantly, ranging from three months to a year, depending on the individual's condition and adherence to the treatment plan.
What role does rehabilitation play in recovery?
Rehabilitation is crucial for recovery. It helps restore function, improve mobility, strengthen supporting muscles, and educate individuals on proper body mechanics to prevent future episodes. It often includes targeted exercises, manual therapy, and posture training.
Are there specific exercises recommended for sciatica relief?
Yes, targeted exercises such as the Piriformis Stretch, Knee-to-Chest Stretch, Bridges, and Cat-Cow Stretch can help alleviate symptoms and strengthen the spine. It's always advisable to consult a healthcare professional before starting any new exercise regimen.
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Understanding Herniated Discs: Herniated discs occur when the inner gel of the disc protrudes, which can compress nearby nerves, leading to pain and discomfort.
- Symptoms of Sciatica: Common symptoms include sharp pain, tingling, or weakness in the legs, often related to herniated discs in the lumbar spine.
- Treatment Options: Treatment can range from physical therapy and exercises to surgical interventions, depending on the severity of the condition.
- Importance of Rehabilitation: Engaging in rehabilitation programs can significantly improve mobility and reduce the risk of future episodes of sciatica.
- Effective Exercises: Targeted exercises like the Piriformis Stretch and Knee-to-Chest Stretch can relieve symptoms and enhance recovery.
- Managing Recovery Expectations: Recovery timelines can vary, and it’s important to maintain realistic expectations and stay consistent with treatment plans.




Stress and Sciatica: Finding Relief
Preparing for Sciatica Surgery: Essentials
Aquatic Therapy for Sciatica Recovery
Exploring Sciatica Medication Options
Ergonomic Solutions for Sciatica Relief